INTRODUCTION
As dental implants continue to be the treatment of choice for many dentists and patients alike, and newer implant systems continue to emerge on the market, the importance of understanding the different implant connections available is imperative for a higher standard of care.
To better understand implant connections, first we have to visualize the timeline of dental implants to see why there is a large variety of connections. Initially, Dr. Gustav Dahl designed subperiosteal implants as a framework placed over the residual ridge with projections resembling abutments as part of the framework for the definitive prosthesis. Later, Dr. Leonard Linkow introduced blade implants that were the first intraosseous implants but similar to a subperiosteal, with the abutment and implant as a unibody. Modern day implants designed by Professor Brånemark were installed for the first patient in 1965, and that was the birth of 2-piece implants and, by extension, implant connections.1
The role of implant connections is to separate the abutment from the implant, thereby allowing us to modify and tailor our treatment methodology in reflection to each clinical presentation with the highest chances of success and survivability. Two-piece implants allow us to modify the design of the prosthesis over time and execute 2-stage surgeries when primary stability is insufficient, achieve primary closure for bone augmentation, and offer an opportunity for further soft tissue manipulation at second-stage surgery. Ultimately, every feature comes with a price; by design, the connection is an interface “microgap” that can be colonized by bacteria, causing bacterial leakage (Figure 1). The interface suffers from micromovements of the abutment under loading, acting as a micro pump for the bacteria into the surrounding tissue. In response, the bone remodels to establish a zone of defense, ie, biologic width. Different interface designs can significantly influence the remodeling of the muco-alveolar complex.2 In response, clinicians and manufacturers poised and developed different designs of implant connections to minimize the drawbacks from a biologic, mechanical, and aesthetic perspective. While the landscape is vast in terms of shapes and sizes, the ideologies and concepts behind the connections are very simple (Table 1).
Figure 1. Microgap at the abutment-implant interface.

The first endosseous-design implants had an external connection. That is the first classification of implant connections: external and internal connections. It is important to note that some scientific papers refer to them as external and internal hex. In this context, “hex” means connection and does not refer to a hexagonal shape (Figure 2).
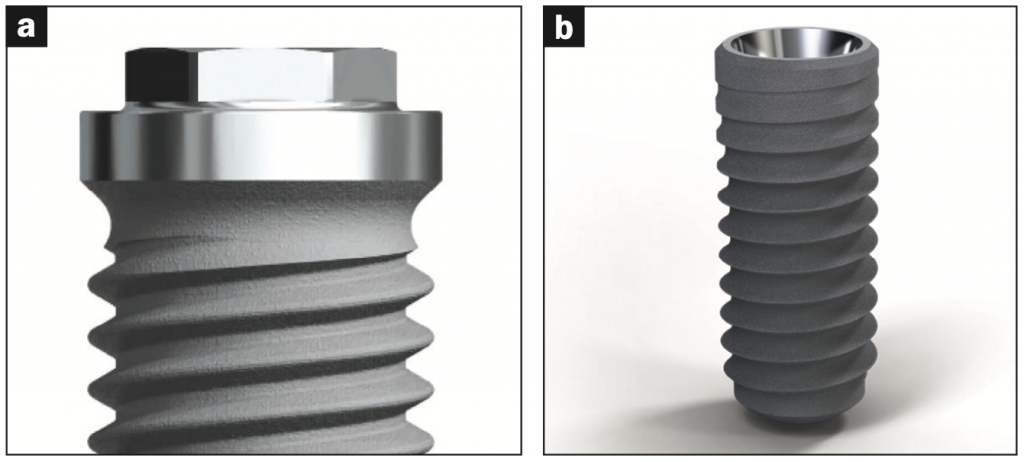
Figure 2. (a) External hex: Brånemark External hex implant (Nobel Biocare). (b) Internal hex: Bone Level Tapered Implant (Straumann).
At that time, implants were used exclusively for full-arch prostheses to restore form and function for completely edentulous patients. The implant installation was followed by a period of 6 months of undisturbed healing; a second-stage surgery for insertion of a transmucosal healing abutment; and, finally, a definitive prosthesis. External connection implants functioned properly without limitations for that purpose, but as their success rates increased, clinicians began expanding their use to off-label indications: partially edentulous and single, missing teeth. Without the rigid fixation and splinting afforded by a full-arch prosthesis, we began experiencing the deficiencies of external connections for single crowns and FPDs: screw loosening (most common), screw fractures, and micromovement at the abutment-implant interface.3 By design, external connections lacked anti-rotation features, had low torquing levels of their prosthetic screws, and a looser fit at the connection level. There are different forms of external hex connections: hexagon, octagon, and spline, and over the years, they have been machined to respond to their inherent problems by adding/increasing friction grips to the hex, deeper screw engagement, wider screw diameters, higher screw torquing levels, and the number of threads.
To overcome the inherent deficiencies of external connections, in 1998, internal connection implants were introduced to assist clinicians in replacing single teeth without external connection implants’ mechanical complications. Internal connections, by design, offered a larger surface area of contact between the abutment and implant as the connection moved inside the implant, improving the fit and minimizing rotational misfit (Figure 3). The longer engagement also created a stiffer, unified interface to resist joint opening, thereby reducing the pumping effect of microleakage and its biological consequences. Additionally, as the connection is bound by the body of the implant, it is able to dissipate the lateral forces within the body of the implants and the investing alveolar bone rather than in the abutment screw.4-7
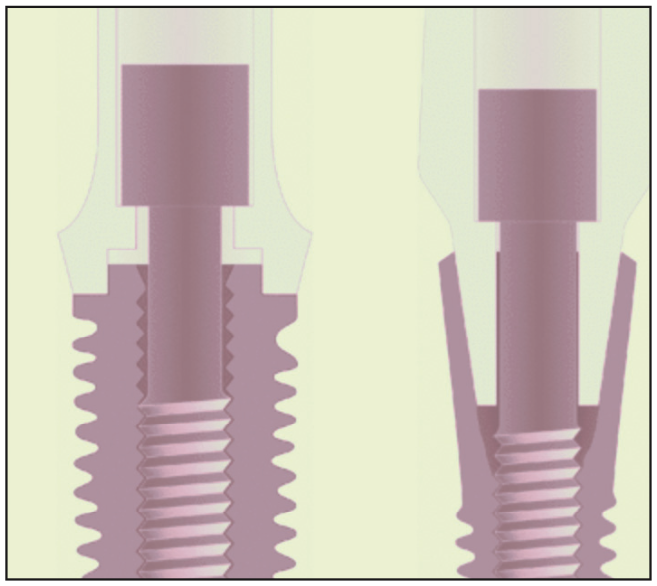
Figure 3. External and internal hex.
The second classification of implant connections derives from the geometric shape of the platform. Many designs exist on the market, most commonly hexagonal, octagonal, conical, trilobe, or a combination of these.8,9 The variety of shapes affords different advantages in terms of passivity, anti-rotation, and microgap size. For example, the mean microgap was significantly larger for flat-to-flat (hexagonal or trilobe) connection systems when compared to conical (ie, Morse taper) connections.10 In true Morse taper connections, the abutment and implant are machined with a specific taper that is press fit together. Oftentimes, the abutments are tapped in rather than held with a screw. While Morse taper fosters the smallest microgap due to the profile and structural design of these connections, the abutments often fracture at the neck of the abutment and are much more difficult to remove when compared to conventional, non-Morse taper connections due to cold welding.11,12 In response, implant manufacturers use a combination of designs to reap the benefits and minimize the drawbacks of different designs with a combination of connection geometry and position. Implants can be categorized as bone-level and tissue-level. Tissue-level implant platforms extend beyond the crest of bone, usually 1.8 to 2.8 mm above the crest with an internal connection. Bone-level implant platforms terminate at the crest of bone and may have an internal or external connection.
The third classification of connections is engaging and non-engaging (Figure 4). Engaging connections, as the term implies, means the abutment has an anti-rotation feature, and the timing of the abutment is important as the definitive final crown can only fit in one specific orientation. With non-engaging abutments, the connection is free to rotate without a specific timing. Engaging abutments have a longer vertical height in the connection and are most commonly used for single crowns. Non-engaging abutments have a shorter vertical height connection and, therefore, are used for multiple-unit and full-arch restorations as it’s easier to have a passive fit of the definitive prosthesis when the implants are not fully parallel.
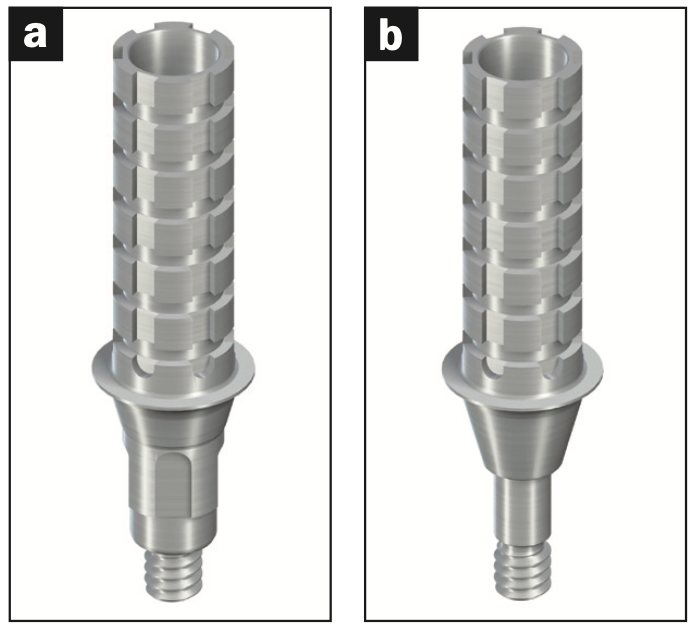
Figure 4. (a) Engaging and (b) non-engaging abutments.
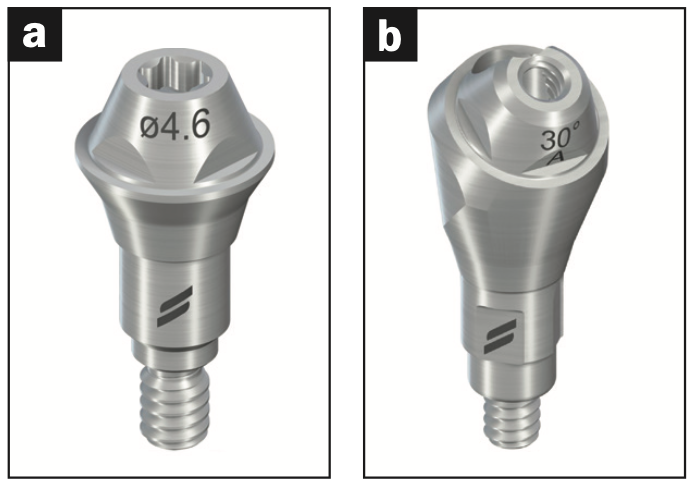
Figure 5. Multi-unit abutments.
The final classification of connections is conventional abutments and multi-unit abutments (MUAs). Conventional abutments have a single screw holding the prosthesis, whether it is screw-retained or cement-retained. MUAs have 2 screws: one screw that holds the MUA onto the implant and another occlusal screw that retains the prosthesis to the MUA (Figure 5). MUAs are used for restorations involving more than one implant and can assist the clinician in correcting for variability in implant angulation and creating a more passive definitive prosthesis.
SUMMARY
As the implant industry continues to evolve, it is essential to recognize that the fundamental principles of implant connections remain unchanged. While this article provides an overview of implant connections, it is not an exhaustive review. Its purpose is to equip readers with a basic understanding that enables them to ask pertinent questions and conduct further research in the field.
REFERENCES
1. Abraham CM. A brief historical perspective on dental implants, their surface coatings and treatments. Open Dent J. 2014;8:50–5. doi:10.2174/1874210601408010050
2. Herrero-Climent M, Romero Ruiz MM, Díaz-Castro CM, et al. Influence of two different machined-collar heights on crestal bone loss. Int J Oral Maxillofac Implants. 2014;29(6):1374–9. doi:10.11607/jomi.3583
3. Meng JC, Everts JE, Qian F, et al. Influence of connection geometry on dynamic micromotion at the implant-abutment interface. Int J Prosthodont. 2007;20(6):623–5.
4. Binon PP. Implants and components: entering the new millennium. Int J Oral Maxillofac Implants. 2000;15(1):76-94.
5. Finger IM, Castellon P, Block M, et al. The evolution of external and internal implant/abutment connections. Pract Proced Aesthet Dent. 2003;15(8):625–32; quiz 634.
6. Sailer I, Sailer T, Stawarczyk B, et al. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int J Oral Maxillofac Implants. 2009;24(5):850–8.
7. Da Silva EF, Pellizzer EP, Quinelli Mazaro JV, et al. Influence of the connector and implant design on the implant-tooth-connected prostheses. Clin Implant Dent Relat Res. 2010;12(3):254–62. doi:10.1111/j.1708-8208.2009.00161.x
8. Coppedê AR, Bersani E, de Mattos Mda G, et al. Fracture resistance of the implant-abutment connection in implants with internal hex and internal conical connections under oblique compressive loading: an in vitro study. Int J Prosthodont. 2009;22(3):283–6.
9. Delgado-Ruiz R, Silvente AN, Romanos G. Deformation of the internal connection of narrow implants after insertion in dense bone: an in vitro study. Materials (Basel). 2019;12(11):1833. doi:10.3390/ma12111833
10. Akça K, Cehreli MC, Iplikçioğlu H. Evaluation of the mechanical characteristics of the implant-abutment complex of a reduced-diameter morse-taper implant. A nonlinear finite element stress analysis. Clin Oral Implants Res. 2003;14(4):444–54. doi:10.1034/j.1600-0501.2003.00828.x
11. Baixe S, Fauxpoint G, Arntz Y, et al. Microgap between zirconia abutments and titanium implants. Int J Oral Maxillofac Implants. 2010;25(3):455–60.
12. Ricciardi Coppedê A, de Mattos Mda G, Rodrigues RC, et al. Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: an in vitro study. Clin Oral Implants Res. 2009;20(6):624–32. doi:10.1111/j.1600-0501.2008.01690.x
ABOUT THE AUTHOR
Dr. Barsoum completed his bachelor’s of dental medicine in 2012 at Misr International University in Cairo. He then graduated magna cum laude from Boston University, where he earned his DMD degree and later completed a 3-year residency and fellowship at New York University in the Ashman Department of Periodontics and Implant Dentistry, where he is also an adjunct assistant professor. Dr. Barsoum’s practice in New York City focuses on dental implants, prosthetics, and full-mouth rehabilitation. He can be reached at adam@barsoum.com or at his practice’s website, nyc.barsoum.com.
Disclosure: Dr. Barsoum reports no disclosures.












