Zirconia puzzle: what makes zirconia unique and how to choose the right zirconia
Zirconia may be part of your everyday vocabulary, but how much do you know about this ceramic material? Learn more…

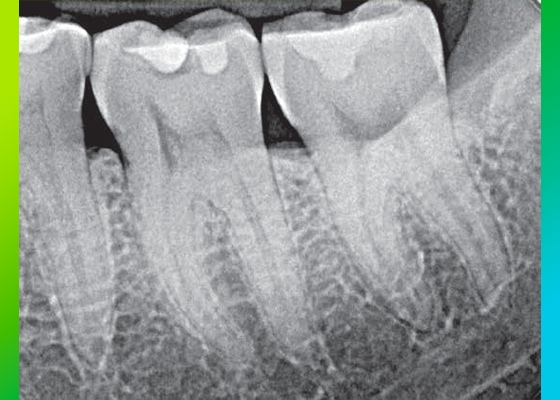
What would you do if you detected radiolucent areas, like the ones shown in Figure 1, under two resin composite restorations in a radiograph? Dental practitioners attending my (Dr. John O. Burgess’) lectures often agree that replacement is the best option, especially if the restoration originates from another dental office.

Fig. 1: Radiolucent areas under resin composite restorations as a result of adhesive pooling.
The reason is quite obvious: Despite a thorough clinical examination, it is impossible to tell if the radiolucency is the result of secondary caries, a lack of marginal adaptation (producing gaps or voids), or simply a thick layer of a radiolucent dental adhesive (Figure 2). Hence, the removal of the existing restoration is the only chance to find the source of the radiolucency immediately. If the adhesive was the cause, nothing will be found underneath the restoration, and overtreatment results. To prevent this possible overtreatment, the dental practitioner needs to monitor the situation and take action only if clinical and radiographic changes are detected during one of the following visits.
The fact that the decision to replace or not to replace a (composite) restoration is often affected by a thick layer of a radiolucent adhesive beneath it has been confirmed in different scientific studies.1,2 The results of an in-vitro study conducted at the Federal University of Santa Maria, Brazil, show that it is twice as likely for a dental practitioner to replace a restoration when there is a dark area visible on a radiograph that is caused by a thick layer of a non-radiopaque dental adhesive.1 Another in-vitro study from Ege University School of Dentistry in Izmir, Turkey, reveals that the use of a radiolucent adhesive leads to a greater number of incorrect radiography-based replacement decisions than the use of a radiopaque adhesive.2

Fig. 2: Possible reasons for radiolucent areas underneath a restoration.
Every dental practitioner leverages the radiopaque effect day in, day out: X-rays are a useful diagnostic tool in dentistry because healthy enamel and dentin offer a certain degree of radiopacity. The effect is caused by hydroxyapatite, or more specifically, the calcium and phosphorous contained in hydroxyapatite, the primary mineral of enamel and dentin. As the hydroxyapatite content is higher in enamel (about 97 percent by weight) than in dentin (about 70 percent by weight)3, enamel appears lighter (more radiopaque) on radiographs. As the amount of hydroxyapatite is significantly reduced in caries-infected tooth structure due to demineralization, carious lesions appear radiolucent (dark) compared to healthy enamel and dentin. Consequently, they can be distinguished from healthy tooth structure on a radiograph.
In order to ensure that dental restorations are distinguishable from these types of defects as well, restorative materials and dental cements are either radiopaque by nature (e.g. amalgam and metal alloys), or made radiopaque by adding specific fillers (e.g. found in composites and luting materials). Most dental adhesives, however, are radiolucent.4,5 This is true of all commercially available universal adhesives launched before September 2020.
Under ideal conditions, dental adhesives form a very thin layer beneath a direct restoration or a thicker layer of resin cement. In an ideal situation, this layer is undetectable by radiographic imaging, so that it might be concluded that adding radiopacity to dental adhesives is simply not necessary. However, in the clinical environment, increased layer thickness and adhesive pooling do occur, not as a result of malpractice, but often due to the force of gravity. Pooling is likely to occur in cavity pits and corners. The layer thickness in pooled areas tends to increase with the filler content of the applied adhesive2 and with multiple coats of the adhesive. However, even unfilled adhesives can produce adhesive pooling with a thickness of more than 40 µm, which is the limit value for detectability of a radiolucent zone on a radiograph.6
Hence, adhesive pooling is a common phenomenon that increases the risk of a misdiagnosis and overtreatment whenever a non-radiopaque dental bonding agent is used. It may occur below a restoration made of composite resin, and also under a layer of radiopaque cement applied in the context of adhesive cementation. Consequently, not only restorative materials and cements, but also adhesives should offer a certain degree of radiopacity to make them distinguishable from secondary caries or gaps and voids at the tooth-restoration interface. The adhesive’s level of radiopacity should be at least equal to that of sound dentin (and at the same level as the radiopacity of an identically thick sample of aluminum), which makes it distinguishable from caries-infected areas.4,7
While adding inorganic radiopaque fillers to restorative materials and dental cements is an adequate solution, this strategy causes problems with dental adhesives. Low or unfilled, low-viscosity adhesives offer the best properties with respect to wetting and penetration of the prepared tooth structure, and therefore ensure a good adaptation to the cavity walls.2 The addition of radiopaque fillers to the formulation would lead to an increase in viscosity, and thus have an impact on the material’s handling properties and adaptation. Another effect is that the fillers separate from the monomers in the adhesive, and the bottle needs shaking before use. If shaking is forgotten or not done properly, adhesive properties like viscosity, handling, wetting behavior, bond strength and radiopacity will vary strongly, leading to inconsistent results. Hence, the strategy of adding radiopaque fillers works well for high-viscosity dental materials, but not for dental adhesives.
The effect of fillers separating from monomers in an otherwise unfilled composition is comparable to the behavior of sand in a bottle of water. When putting the bottle aside, the sand will settle to the bottom of the bottle. By shaking the bottle thoroughly, the components are mixed, but the sand will start settling again after mixing. The quality of the mixture depends on how well the bottle is shaken, and also on the time elapsing between mixing and the use of the liquid (Figure 3).

Fig. 3: The behavior of sand in water: a) stagnant sand and water in a bottle; b) sand and water immediately after thorough shaking of the bottle; c) situation after several seconds as the sand settles at the bottom.
In order to overcome these issues, 3M developed an improved version of 3M™ Scotchbond™ Universal Adhesive. The new product, 3M™ Scotchbond™ Universal Plus Adhesive, offers the desired dentin-like radiopacity and a low viscosity without the need for shaking before use – eliminating the risk for a settling of particles (Figure 3). 3M accomplished this by developing a new, radiopaque monomer. Its radiopacity is embedded in the monomer, which ensures its homogeneous distribution throughout the material and consistent performance. In addition to the radiopacity feature, the new monomer is not derived from Bisphenol-A. As the radiopaque monomer replaces the BisGMA resin of the original Scotchbond Universal formulation, the formulation of the new Scotchbond Universal Plus Adhesive is free of BPA derivatives.
The radiopacity feature of the new 3M™ Scotchbond™ Universal Plus Adhesive is special in that it does not compromise the product’s performance, while facilitating interpretation of dental radiographs whenever adhesive pooling occurs. In this way, one can reduce guesswork diagnosing dental restoration replacement in daily clinical practice – and prevent overtreatment in many cases whenever adhesive pooling occurs (Figure 4).
It is of course important to keep in mind that X-rays are always only complementary to a clinical examination, as radiolucency can have many causes, including X-ray artifacts.

Fig. 4: Provoked adhesive pooling produces radiolucent areas that might lead to a misdiagnosis with three different universal adhesives. Due to its radiopacity, 3M™ Scotchbond™ Universal Plus Adhesive blends in well with the surrounding dentin, so that interpretation of this radiograph is much less challenging.8
References

Zirconia may be part of your everyday vocabulary, but how much do you know about this ceramic material? Learn more…

Achieving the correct shape is vital to a natural-looking anterior composite restoration. Learn how the 3M™ Filtek™ Matrix, paired with…

Direct composite restorative procedures can be challenging, particularly when it comes to esthetic cases. Discover how new techniques and tools…