INTRODUCTION
Implant dentistry research has demonstrated high success rates in the reconstruction of partial and fully edentulous sites.1 The placement of implants into fresh extraction sockets, known as immediate implant placement (IIP), was first described more than 50 years ago.2,3 Today, it is widely accepted by the clinical community because IIP shares comparable survival rates to those of implants placed in healing sockets.4-7 The IIP approach can streamline the surgical and prosthetic stages, reducing appointments and overall treatment time.8 Extended treatment times may impact patient decisions toward faster treatment rather than ideal treatment.
IIP in the posterior maxilla requires an in-depth knowledge of several surgical and prosthetic techniques. The approach includes extraction, implant placement, final impression taking, guided bone regeneration, and placement of an implant restoration. In addition, sinus augmentation and growth factors in platelet concentrates may be needed as part of the skill set of the clinician to enhance hard- and soft-tissue healing.9-11
After an osseointegration period, the final abutment and restoration are placed. The entire process is completed in 2 appointments, including a single surgery within a 3- to 4-month time interval. The time period prior to loading is determined by several factors, including bone quality and quantity, biomechanics, and occlusion. IIP in the posterior maxillary molar sites is more challenging than using this approach in single-rooted teeth.12
This article discusses a specific approach for the management of a maxillary molar with a poor prognosis. The IIP case demonstrates the surgical and prosthetic protocol for a posterior maxillary molar tooth. Research discussing this clinical scenario is limited in the body of evidence.
CASE REPORT
A 58-year-old female patient was referred by an endodontist for extraction and a restorative treatment plan. A diagnosis of apical periodontitis with a vertical root fracture was made for the maxillary left first molar (tooth No. 14). The clinical and radiographic evaluation demonstrated an existing porcelain-fused-to-metal crown and previous endodontic therapy. The periapical and CBCT imaging revealed a large periapical radiolucency (Figures 1 to 3).
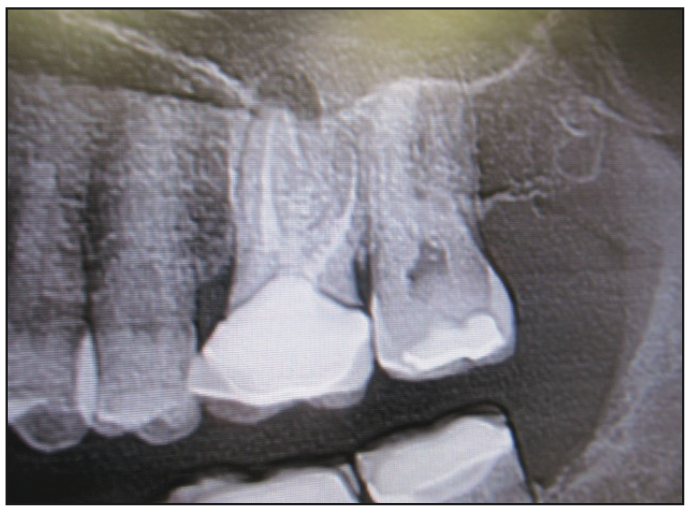
Figure 1. Periapical radiograph of the maxillary left first molar (tooth No. 14).
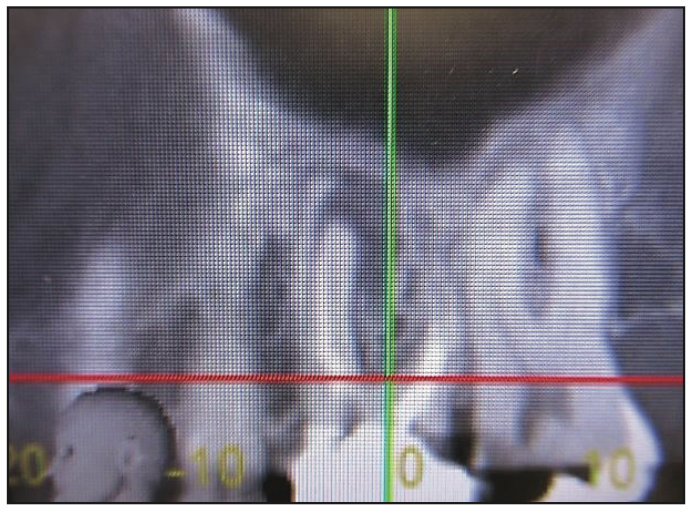
Figure 2. CBCT image, sagittal view.

Figure 3. CBCT image, sagittal view.
The surgical phase was initiated with a 20-mL whole blood draw via the median cubital vein. Buffy coat platelet-rich plasma (BC-PRP) and platelet-rich fibrin (PRF) were produced in a single spin centrifuge, centrifuged at 3,100 rpm for 12 minutes, and processed (Figure 4). Local anesthesia (1 carpule 3% Polocaine without epinephrine [54 mg] and 1 carpule 4% Articaine with 1:100,000 epinephrine [72mg] [Benco Dental]) was administrated. An intrasulcular incision utilizing a 15c blade was made. Then Nos. 1 and 2 periotomes, and sectioning of the mesial/buccal, distal/buccal, and palatal roots with a No. 4 long shank round bur were performed. A universal forceps was used to remove 3 individual roots, followed by thorough debridement of the tooth socket with a double-ended molt curette and irrigation with 10% Povidone solution.

Figure 4. Platelet-rich fibrin.
A 4.7- × 13-mm SBM tapered implant (Legacy1 [Implant Direct]) was placed with a straight driver. Prior to implant placement, the osteotomy and internal sinus augmentation were performed with Densah osseodensification drills (OD) (Versah [Huwais IP Holding]) (Figure 5). A 1.6-mm pilot drill rotating clockwise (forward) initiated the osteotomy, followed by 2.0-, 2.5- and 3.0-mm Densah drills rotating in a counterclockwise (reverse) movement. The final OD drill size was 4.0 mm in diameter and extended 2 mm apical to the sinus floor. A PRF bioactive plug was placed in the osteotomy, followed by a mixture of BC-PRP and mineralized irradiated bone allograph (perio [Rocky Mountain Tissue Bank]). The grafting materials utilized in the crestal (internal) sinus augmentation were introduced into the osteotomy with a 3.8-mm straight osteotome. A fixture-level impression was taken with a 4.7-mm concave transfer pin. Following the impression, the transfer pin was removed and replaced with a 4.7- × 3-mm healing collar. The gap space between the implant surface and socket wall was grafted with BC-PRP and mineralized irradiated bone allograph (Rocky Mountain Tissue Bank) of fine particle size ranging from 250 to 1,000 µm. The graft material was placed in the gingival sulcus up to the free gingival margin. A non-resorbable d-PTFE barrier (Cytoplast [Implant Direct]) was secured over the healing collar with 4.0 Vicryl sutures, and a periapical radiograph was taken (Figures 6 and 7).
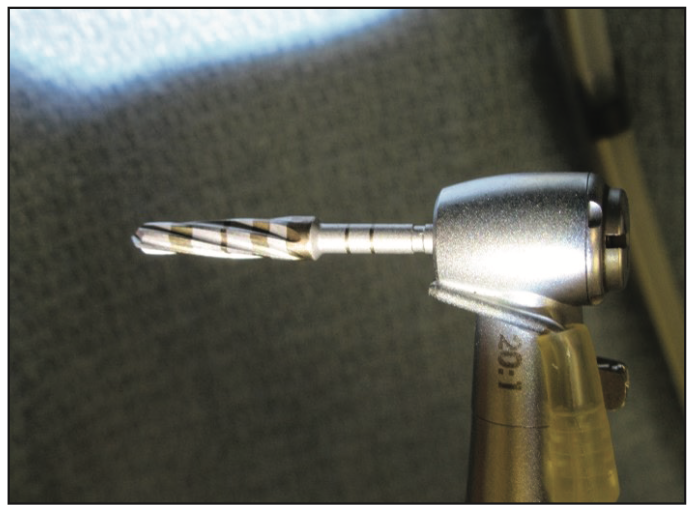
Figure 5. A 3.0-mm Densah drill (Versah).

Figure 6. A d-PTFE non-resorbable barrier.

Figure 7. Periapical radiograph of the fixture/healing collar.
After 4 months, the healing collar was removed (Figure 8). A titanium abutment was placed utilizing an orientation jig and was followed by a periapical radiograph (Figures 9 and 10). The abutment screw was torqued to 30 N/cm 2 times at 5-minute intervals (Figure 11). The definitive PFM crown was placed with a permanent cement (Zinc Phosphate [Bosworth Co]) (Figures 12 and 13).

Figure 8. Healing collar.

Figure 9. Orientation jig.

Figure 10. Periapical radiograph, abutment.

Figure 11. Titanium abutment.

Figure 12. Final prosthesis, porcelain-fused-to-metal crown (occlusal view).

Figure 13. Final prosthesis, porcelain-fused-to-metal crown (facial view).
DISCUSSION
The IIP approach differs from the conventional implant surgical approach employed since the inception of endosseous implant therapy. However, IIP demonstrates similar success rates of greater than 98% to the staged implant approach. Recently, the IIP approach in the posterior maxilla has been more widely utilized because of innovative instrumentation, implant design, and surface characteristics.13 IIP procedures are more challenging in the posterior maxillary regions due to the quality and quantity of bone, as well as the presence of anatomical structures. However, the majority of IIP principles and protocols are similar with subtle differences depending on whether they are utilized in the anterior or posterior region of the mouth.
The surgical aspect of IIP in the maxillary molar region is initiated with a flapless, atraumatic extraction of the tooth. It is accomplished by expansion of bone, sectioning, and removal of 3 individual root fragments. This extraction approach allows for the removal of the tooth while maintaining the bone volume needed for primary fixation of the implant body. Primary fixation is the primary objective of the implant surgical placement stage. The ideal position and stability of the implant can be best achieved utilizing a CBCT-generated guide or ODs or by preparing the osteotomy through the residual root.14-16 The trajectory of the osteotomy is in an apical-palatal direction to enhance primary stability.17
Implant surgical placement in the posterior maxillary aspect often requires simultaneous sinus augmentation. Osseodensification instrumentation facilitates the expansion of soft bone and a reduction in membrane perforations, which enhance positive outcomes.18 The osseodensification technique has demonstrated an increase in implant primary stability, bone mineral density, and the preservation of bone at the implant surface. Osseodensification preserves bone volume through compaction of cancellous bone due to the natural properties of viscoelasticity and plastic deformation.19 Primary stability and preservation of bone bulk in low-density bone and the reduction in micromotion directly impacts the healing process.20,21
A torque value greater than 45 N/cm is not required in the molar region, only a lack of movement or spinning of the implant fixture because a provisional crown is usually utilized in the anterior or aesthetic zone. A healing collar is placed over the fixture in the posterior non-aesthetic zone during the osseointegrative phase.
The gap that exists between the socket wall and implant surface can be managed with various procedures and materials. Platelet concentrates and allographic bone are common components associated with a crestal (internal) sinus augmentation and gap management. A single platelet contains more than 1,000 growth factors, including platelet-derived growth factor, transferring growth factors beta 1 and 2, and endothelial vascular growth factors. Growth factors have exhibited an increase in the recruitment, differentiation, and quantity of cells associated with tissue healing. BC-PRP is mixed with allographs to serve as a carrier or with PRF as a bioactive membrane for cell development. Allographic cadaver bone is commonly utilized in IIP due to its available quantities, safety, and osseoconductive properties.22,23 In addition, allographic bone serves as an osseinductive source via bone morphogenic protein. A particle size of 250 to 1,000 µm used in this study was obtained from a human vertebral source and gamma-irradiated at 2.5 to 3.8 mrad to kill all bacteria, viruses, and cells.24,25 Allogenic graft is made of scaffolds from human cadavers and processed to maintain structure and extracellular protein.26 It is packaged in a hydrated form to increase strength and flexibility.27 Studies have demonstrated that grafting the gap increases hard tissue.28 Studies demonstrate that graft materials coronal to the implant platform to the free gingival margin enhance the thickness of soft tissue. Graft materials may alter the biotype or reduce the likelihood of a connective tissue graft.29
The restorative stage is initiated at the surgical appointment with a fixture-level impression. The impression can be taken with predictable results based on primary stability, proper 3D implant placement, and graft material placement in the gap as well as coronal to the connection to the top of the healing collar. The final restoration is delivered after an osseointegration period. A standard titanium abutment is placed, and its retaining screw is torqued to the appropriate value 2 times in a 5-minute time interval to ensure an intimate fit.30 The final PFM restoration is placed with a permanent cement.
Implant occlusal principles for the final restoration should exhibit zero contact during central occlusion, excursions, or protrusion. The buccal/palatal dimension of the occlusal table is reduced to mimic the size of a premolar. Occlusal table width is directly related to the applied force to the crest of bone. Therefore, a reduction in B/P dimension minimizes the force applied to the crest of the bone.31
ACKNOWLEDGMENTS
The author wishes to acknowledge Tatyana Lyubezhanina, DA, and LeeAnn Klotz, DA, for their assistance in preparation of this article.
REFERENCES
1. Albrektsson T, Brånemark PI, Hansson HA, et al. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155–70. doi:10.3109/17453678108991776
2. Schulte W, Heimke G. Das Tübinger Sofort-Implant [The Tübinger immediate implant]. Quintessenz. 1976;27(6):17-23. German.
3. Schulte W, Kleineikenscheidt H, Lindner K, et al. Das Tübinger Sofortimplantat in der klinischen Prüfung [The Tübingen immediate implant in clinical studies]. Dtsch Zahnarztl Z. 1978;33(5):348–59. German.
4. Quirynen M, Van Assche N, Botticelli D, et al. How does the timing of implant placement to extraction affect outcome? Int J Oral Maxillofac Implants. 2007;22 Suppl:203–23. Erratum in: Int J Oral Maxillofac Implants. 2008;23(1):56.
5. Schropp L, Isidor F. Timing of implant placement relative to tooth extraction. J Oral Rehabil. 2008;35(Suppl 1):33-43. doi:10.1111/j.1365-2842.2007.01827.x
6. Becker W, Goldstein M. Immediate implant placement: treatment planning and surgical steps for successful outcome. Periodontol 2000. 2008;47:79-89. doi:10.1111/j.1600-0757.2007.00242.x
7. Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009;24(Suppl):186-217.
8. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9(5):332–43.
9. Jackson BJ. Proposed treatment approach for type II sockets: report of two cases. J Oral Implantol. 2019;45(3):227–34. doi:10.1563/aaid-joi-D-18-00148
10. Summers RB. The osteotome technique: Part 3—Less invasive methods of elevating the sinus floor. Compendium. 1994;15(6):698-704.
11. Rutkowski JL, Thomas JM, Bering CL, et al. An analysis of a rapid, simple, and inexpensive technique used to obtain platelet-rich plasma for use in clinical practice. J Oral Implantol. 2008;34(1):25-33. doi:10.1563/1548-1336(2008)34[25:AAOARS]2.0.CO;2
12. Atieh MA, Payne AG, Duncan WJ, et al. Immediate placement or immediate restoration/loading of single implants for molar tooth replacement: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2010;25(2):401–15.
13. Lang NP, Pun L, Lau KY, et al. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res. 2012;23(Suppl 5):39-66. doi:10.1111/j.1600-0501.2011.02372.x
14. Schneider D, Marquardt P, Zwahlen M, et al. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res. 2009;20(Suppl 4):73-86. doi:10.1111/j.1600-0501.2009.01788.x
15. Davarpanah M, Szmukler-Moncler S. Unconventional implant treatment: I. Implant placement in contact with ankylosed root fragments. A series of five case reports. Clin Oral Implants Res. 2009;20(8):851–6. doi:10.1111/j.1600-0501.2008.01653.x
16. Rebele SF, Zuhr O, Hürzeler MB. Pre-extractive interradicular implant bed preparation: case presentations of a novel approach to immediate implant placement at multirooted molar sites. Int J Periodontics Restorative Dent. 2013;33(1):89-96. doi:10.11607/prd.1444
17. Lang NP, Berglundh T; Working Group 4 of Seventh European Workshop on Periodontology. Periimplant diseases: where are we now? Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol. 2011;38(Suppl 11):178–81. doi:10.1111/j.1600-051X.2010.01674.x
18. Huwais S, Meyer EG. A novel osseous densification approach in implant osteotomy preparation to increase biomechanical primary stability, bone mineral density, and bone-to-implant contact. Int J Oral Maxillofac Implants. 2017;32(1):27-36. doi:10.11607/jomi.4817
19. Pikos MA, Miron RJ. Osseodensification: An Overview of Scientific Rationale and Biological Background. Compend Contin Educ Dent. 2019;40(4):217–22.
20. Trisi P, Berardini M, Falco A, et al. New osseodensification implant site preparation method to increase bone density in low-density bone: in vivo evaluation in sheep. Implant Dent. 2016;25(1):24-31. doi:10.1097/ID.0000000000000358
21. Tabassum A, Meijer GJ, Walboomers XF, et al. Evaluation of primary and secondary stability of titanium implants using different surgical techniques. Clin Oral Implants Res. 2014;25(4):487–92. doi:10.1111/clr.12180
22. Amstutz HC, Sissons HA. The structure of the vertebral spongiosa. J Bone Joint Surg Br. 1969;51(3):540–50.
23. Elsharkawy AT, Sharaqy M, Beheiry MG, et al. Autologous versus allogeneic bone blocks for augmentation of maxillary deficiency. Egypt Dent J. 2013;59:4117–21.
24. Tatum OH Jr, Lebowitz MS, Tatum CA, et al. Sinus augmentation. Rationale, development, long-term results. N Y State Dent J. 1993;59(5):43–8.
25. Tatum OH Jr. Osseous grafts in intra-oral sites. J Oral Implantol. 1996;22(1):51–2.
26. Troeltzsch M, Troeltzsch M, Kauffmann P, et al. Clinical efficacy of grafting materials in alveolar ridge augmentation: A systematic review. J Craniomaxillofac Surg. 2016;44(10):1618–29. doi:10.1016/j.jcms.2016.07.028
27. Pabst A, Ackermann M, Thiem D, et al. Influence of different rehydration protocols on biomechanical properties of allogeneic cortical bone plates: a combined in-vitro/in-vivo study. J Invest Surg. 2021;34(10):1158–64. doi:10.1080/08941939.2020.1767735. Erratum in: J Invest Surg. 2020;1-2
28. Araújo MG, Linder E, Lindhe J. Bio-Oss collagen in the buccal gap at immediate implants: a 6-month study in the dog. Clin Oral Implants Res. 2011;22(1):1-8. doi:10.1111/j.1600-0501.2010.01920.x
29. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524–32, 534.
30. Winkler S, Ring K, Ring JD, et al. Implant screw mechanics and the settling effect: overview. J Oral Implantol. 2003;29(5):242–5. doi:10.1563/1548-1336(2003)029<0242:ISMATS>2.3.CO;2
31. Misch CE. Chapter 31: Occlusal considerations for implant-supported prosthesis. In: Misch CE, ed. Contemporary Implant Dentistry. 2nd ed. Mosby; 1993:705–33.
ABOUT THE AUTHOR
Dr. Jackson graduated from Utica University with a BS degree in biology, cum laude. He received his DDS degree at the State University of New York at Buffalo School of Dental Medicine. Dr. Jackson completed postgraduate training at St. Luke’s Memorial Hospital Center’s General Practice Residency Program. He completed his formal implant training through the New York Maxicourse in Oral Implantology at the New York University College of Dentistry. He is board-certified and a Diplomate of the American Board of Oral Implantology/Implant Dentistry and an Honored Fellow of the American Academy of Implant Dentistry (AAID). Dr. Jackson is the past president of the AAID. He is an attending staff dentist for Faxton-St. Luke’s Healthcare General Practice Residency Program. He is a member of the ADA and director of the AAID Boston Maxicourse in Oral Implantology and the East Coast Implant Institute. Dr. Jackson has published several articles in peer-reviewed journals on the topic of oral implantology and implant dentistry. He can be reached at bjjddsimplant@aol.com.
Disclosure: Dr. Jackson reports no disclosures.











